Intelligent ePrescribing Overview
Payers support various levels of ePrescribing, while it is difficult to know which level of support each payer provides. The Intelligent ePrescribing solutions delivers information to ensure patients get the most cost effective, clinically appropriate medication.
Although EHRs may have different layout, the information is typically displayed within your EHR.
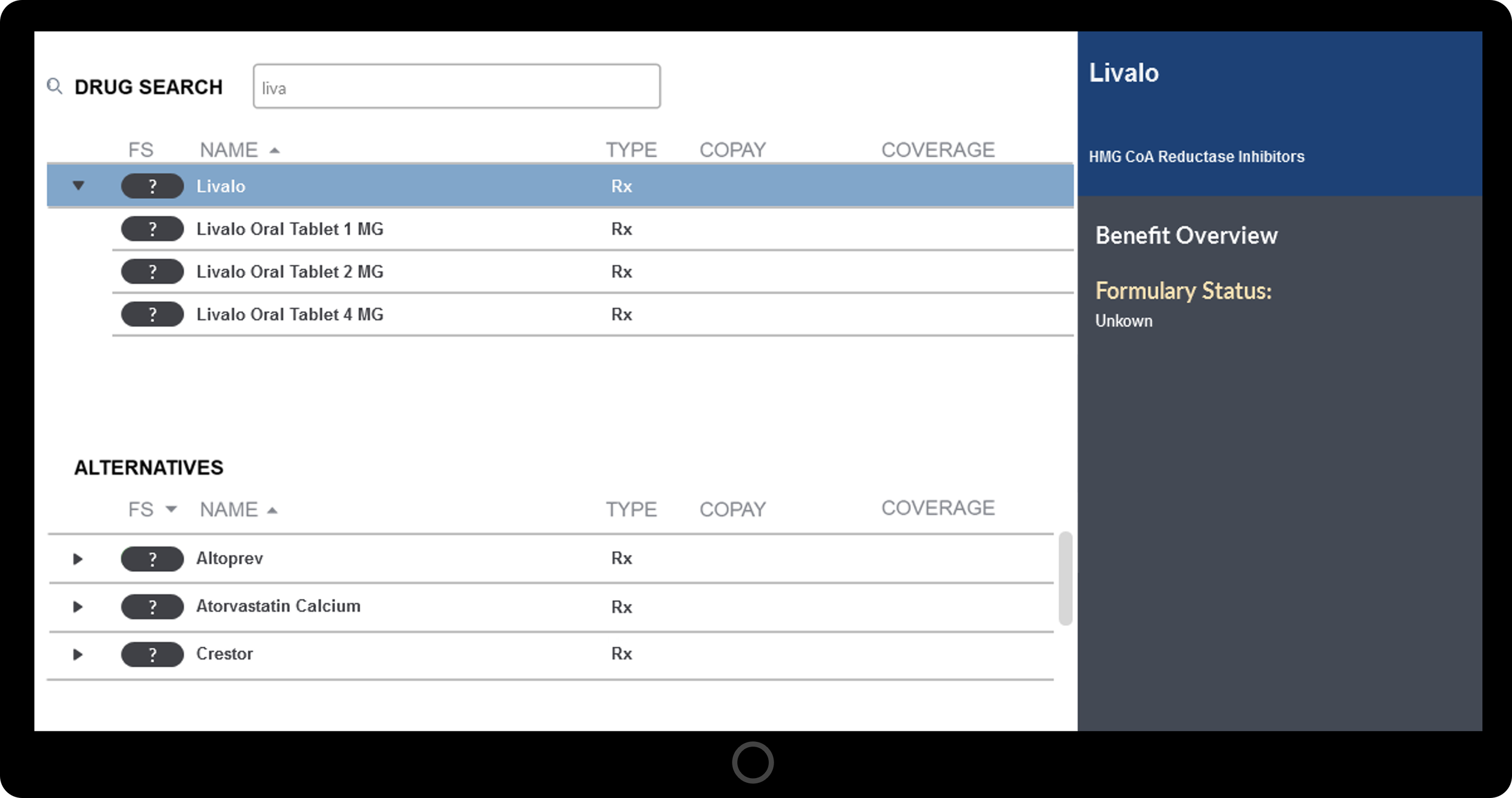
ePrescribing without Formulary & Benefit Information
Without the Intelligent ePrescribing solution, Formulary & Benefit (F&B) information is not supported such that the status, copay and coverage is non-existent. In addition, alternatives are most often not available for therapeutic class drug lists.
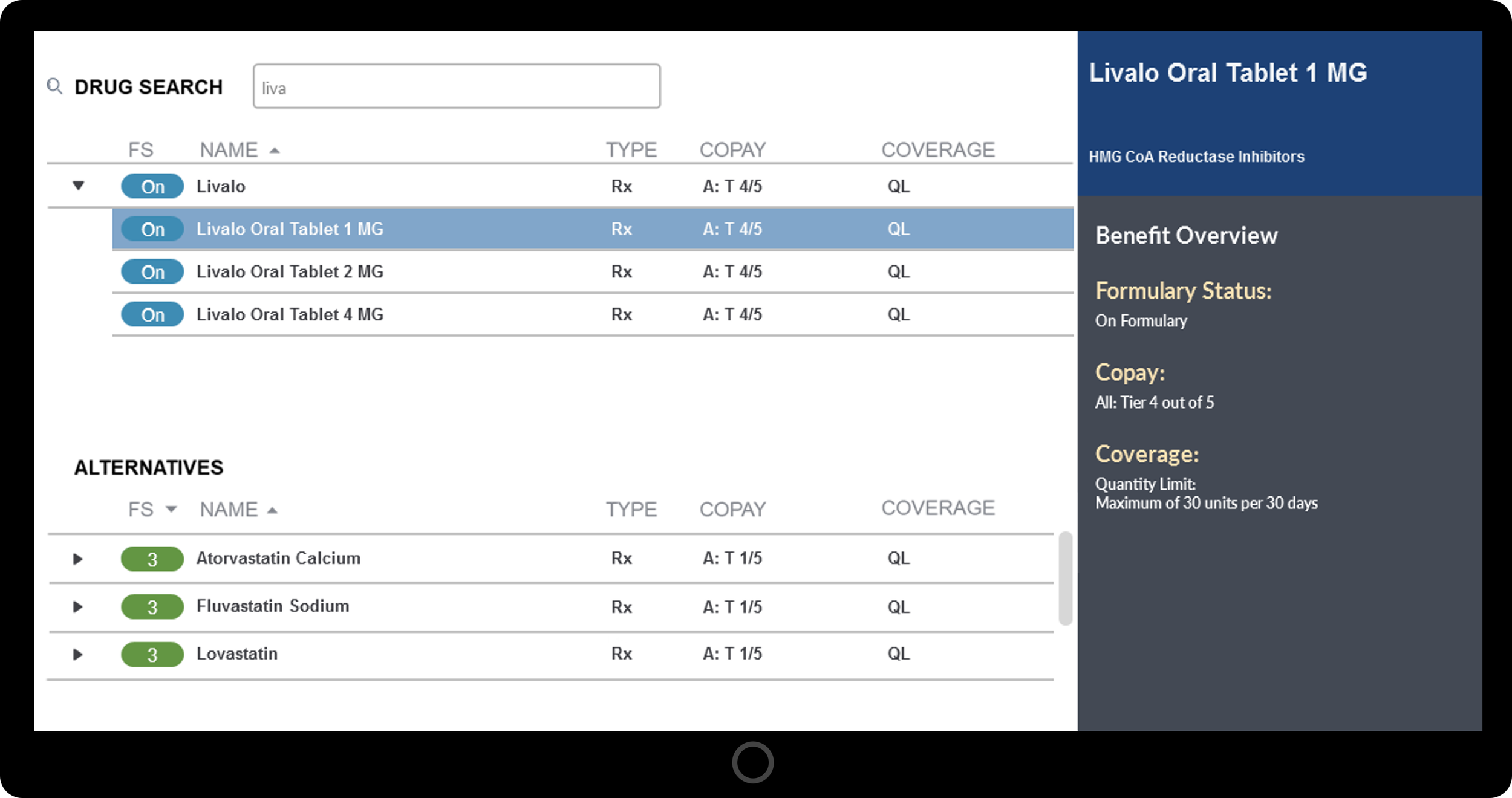
ePrescribing with basic Formulary & Benefit Information
With only basic F&B information, formulary status is displayed showing preferred as a colored number; “P1 or Preferred (lvl 1) or Preferred level 1,” non-formulary / not preferred; non-formulary or not covered.
Copay is displayed as a tier reflecting the relative cost or formulary status value. Most often tiers are stated as Tier X out of the max tier value (e.g. Tier 1 out of 5) with lower tier values being better.
Coverage information at this level of detail supports prior authorization, step therapy indicator, quantity limits, and some messaging. Alternatives are sorted by therapeutic class as determined by the source drug compendia and formulary status, while being displayed alphabetically.
ePrescribing with enhanced Formulary & Benefit Information
With enhanced F&B, detailed information including Intelligent ePrescribing SmartAlts™ are shown. This includes formulary status displays in the form of a colored number; “P1 or Preferred (lvl 1) or Preferred level 1,” non-formulary / not preferred; non-formulary or not covered.
Copay is shown in a more detailed manner including flat dollar copay (e.g. $5), percentage copay (e.g. 100% or 25% with a minimum copay of $25 and a maximum copay of $250), day supply based on the copay amount are often displayed, and copays varying depending on 30 day versus 90 day and 90 day retail versus 90 day main order.
Coverage information at this level of detail supports prior authorization, step therapy indicator, quantity limits, age limits, gender limits, explicit step medication lists, and messaging such as text-based or web link. And finally, a list of therapeutically similar SmartAlts™ drugs are sorted by formulary status and price.